دوره 28، شماره 3 - ( دوماهنامه طب جنوب 1404 )
جلد 28 شماره 3 صفحات 743-724 |
برگشت به فهرست نسخه ها
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Mazarei Z, Hamidi A, Ravanipour M, Omrani A, Ravanipour M. Endocrine Disruptors and Attention Deficit Hyperactivity Disorder: A Systematic Review of Environmental Monitoring Exposure Studies. Iran South Med J 2025; 28 (3) :724-743
URL: http://ismj.bpums.ac.ir/article-1-2345-fa.html
URL: http://ismj.bpums.ac.ir/article-1-2345-fa.html
مزارعی زهرا، حمیدی علی، روانیپور مریم، عمرانی عبدالمجید، روانیپور معصومه. مختلکنندههای اندوکرینی و مشکلات کمبود توجه- بیشفعالی: یک مرور نظاممند بر مطالعات پایش محیطی مواجهه. مجله طب جنوب. 1404; 28 (3) :724-743
زهرا مزارعی1 

 ، علی حمیدی2
، علی حمیدی2 
 ، مریم روانیپور3
، مریم روانیپور3 
 ، عبدالمجید عمرانی4
، عبدالمجید عمرانی4 
 ، معصومه روانیپور*5
، معصومه روانیپور*5 




 ، علی حمیدی2
، علی حمیدی2 
 ، مریم روانیپور3
، مریم روانیپور3 
 ، عبدالمجید عمرانی4
، عبدالمجید عمرانی4 
 ، معصومه روانیپور*5
، معصومه روانیپور*5 


1- گروه پزشکی عمومی، دانشکده پزشکی، دانشگاه علوم پزشکی بوشهر، بوشهر، ایران
2- گروه کتابداری پزشکی، دانشکده پیراپزشکی، دانشگاه علوم پزشکی بوشهر، بوشهر، ایران
3- گروه پرستاری، دانشکده پرستاری و مامایی، دانشگاه علوم پزشکی بوشهر، بوشهر، ایران
مرکزتحقیقات طب گرمسیری و عفونی خلیجفارس، پژوهشکده علوم زیست پزشکی خلیجفارس، دانشگاه علوم پزشکی بوشهر، بوشهر، ایران
4- گروه کودکان، دانشکده پزشکی، دانشگاه علوم پزشکی بوشهر، بوشهر، ایران
5- گروه مهندسی بهداشت محیط، دانشکده بهداشت و تغذیه، دانشگاه علوم پزشکی بوشهر، بوشهر، ایران ،ravan.mas@gmail.com
2- گروه کتابداری پزشکی، دانشکده پیراپزشکی، دانشگاه علوم پزشکی بوشهر، بوشهر، ایران
3- گروه پرستاری، دانشکده پرستاری و مامایی، دانشگاه علوم پزشکی بوشهر، بوشهر، ایران
مرکزتحقیقات طب گرمسیری و عفونی خلیجفارس، پژوهشکده علوم زیست پزشکی خلیجفارس، دانشگاه علوم پزشکی بوشهر، بوشهر، ایران
4- گروه کودکان، دانشکده پزشکی، دانشگاه علوم پزشکی بوشهر، بوشهر، ایران
5- گروه مهندسی بهداشت محیط، دانشکده بهداشت و تغذیه، دانشگاه علوم پزشکی بوشهر، بوشهر، ایران ،
چکیده: (663 مشاهده)
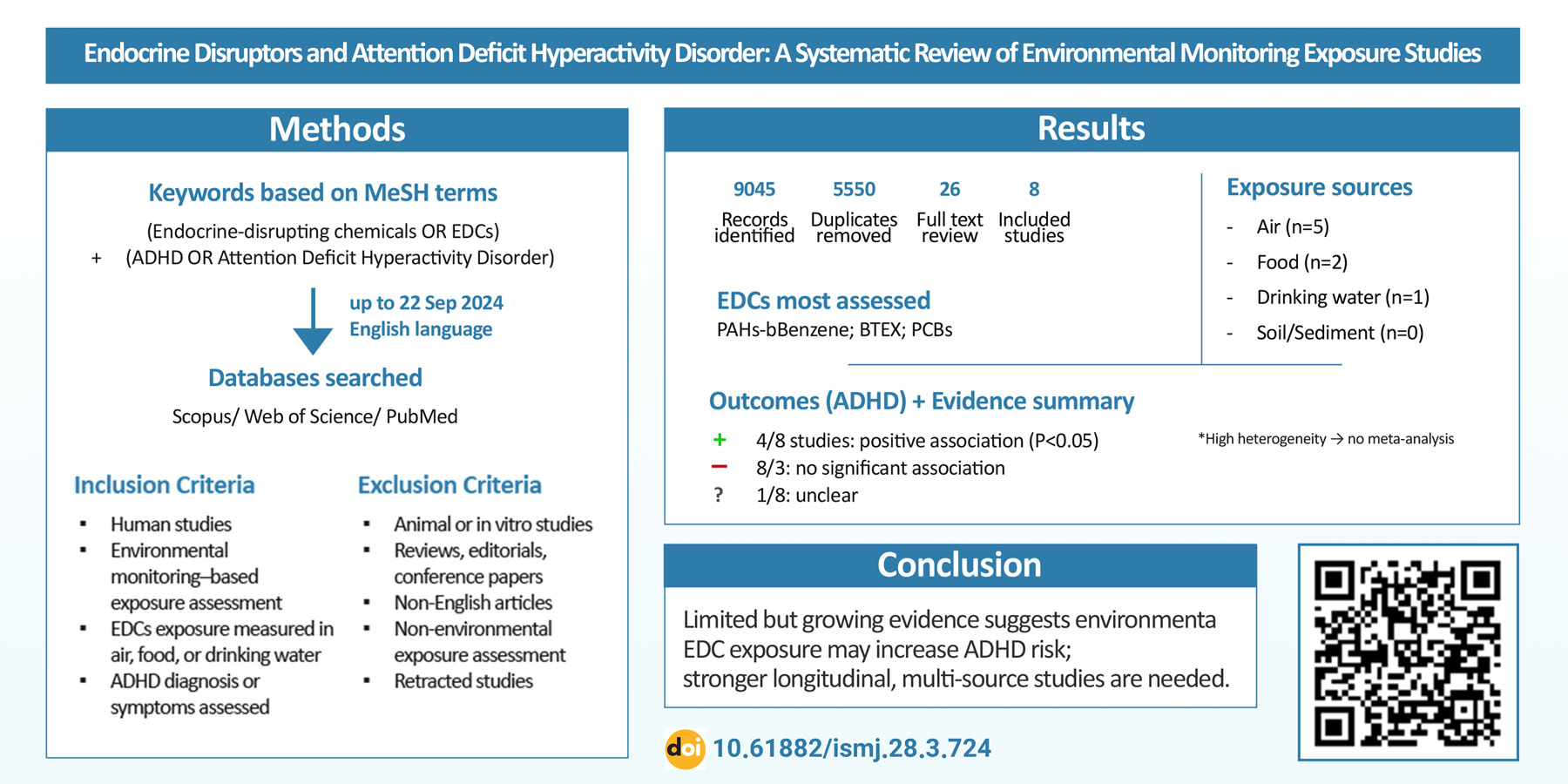
زمینه: اختلال کمبود توجه- بیشفعالی (ADHD) یکی از شایعترین اختلالات عصبی- رشدی در کودکان است که علتشناسی آن چندعاملی و پیچیده است. شواهد اخیر حاکی از نقش ترکیبی عوامل، بهویژه ترکیبات شیمیایی مختلکننده غدد درونریز (EDCs)، بهعنوان عوامل محیطی مؤثر در بروز این اختلال از طریق برهمزدن مسیرهای تنظیم هورمونی و رشد عصبی است. با وجود رشد مطالعات در این حوزه، هنوز شواهد کافی درباره رابطه بین مواجهه محیطی با EDCها (بر اساس پایش محیطی) و بروز ADHD وجود ندارد. از اینرو، این مرور نظاممند با هدف تعیین شواهد موجود درباره ارتباط بین مواجهه از طریق پایش محیطی با EDCها و بروز علائم ADHD انجام شد.
مواد و روشها: مطالعه حاضر یک مرور نظاممند انجام شده مطابق با چکلیست پرایزما میباشد. تمامی مقالات پژوهشی به زبان انگلیسی بدون محدودیت زمانی چاپ تا ۲۲ سپتامبر ۲۰۲۴ میلادی در سه پایگاه داده Scopus، Web of Science و PubMed با استفاده از کلیدواژههای مرتبط با موضوع و بر اساس اصطلاحاتMeSH جستجو شدند. تمامی مراحل غربالگری مقالات بر اساس معیارهای ورود و خروج انجام شد. در نهایت، دادههای مورد نیاز از مقالات نهایی بازیابی شده، استخراج شد.
یافتهها: از میان ۹۰۴۵ نتیجه جستجو، با حذف ۳۴۹۵ مورد تکراری و پس از بررسی کامل متون در نهایت ۸ مقاله برای تحلیل نهایی انتخاب شدند. بیشترین دامنه انتشار مقالات منتخب در ۱۰ سال اخیر بودند و از نظر منابع مواجهه بهترتیب هوا، غذا و آب شرب شایعترین منبع بررسی شده بودند، در حالیکه برای خاک و رسوبات هیچ مطالعهای یافت نشد. بیشترین آلایندههای مورد ارزیابی شامل PAHها، بنزن و BTEX بودند. در حدود نیمی از مطالعات، ارتباط مثبت و معنیدار بین مواجهه با برخی از EDCها و بروز علائم ADHD گزارش شد، در حالیکه سایر مطالعات چنین ارتباطی را نیافتند.
نتیجهگیری: یافتههای این مرور نشان میدهد که اگرچه شواهد رو به رشدی از ارتباط بالقوه بین مواجهه محیطی با EDCها و افزایش خطر ADHD وجود دارد، اما تعداد مطالعات محدود و وجود برخی ناهمگنیها مانع از نتیجهگیری قطعی میشود. این مطالعه ضرورت طراحی پژوهشهای آینده با رویکرد طولی و ارزیابی مواجهه چندمنبعی با کنترل متغیرهای مخدوشکننده را برجسته میسازد. همچنین، توجه به منابع کمتر بررسیشده مانند خاک و رسوبات میتواند به درک جامعتر از مسیرهای واقعی مواجهه و پیامدهای رشد عصبی کودکان کمک کند.
مواد و روشها: مطالعه حاضر یک مرور نظاممند انجام شده مطابق با چکلیست پرایزما میباشد. تمامی مقالات پژوهشی به زبان انگلیسی بدون محدودیت زمانی چاپ تا ۲۲ سپتامبر ۲۰۲۴ میلادی در سه پایگاه داده Scopus، Web of Science و PubMed با استفاده از کلیدواژههای مرتبط با موضوع و بر اساس اصطلاحاتMeSH جستجو شدند. تمامی مراحل غربالگری مقالات بر اساس معیارهای ورود و خروج انجام شد. در نهایت، دادههای مورد نیاز از مقالات نهایی بازیابی شده، استخراج شد.
یافتهها: از میان ۹۰۴۵ نتیجه جستجو، با حذف ۳۴۹۵ مورد تکراری و پس از بررسی کامل متون در نهایت ۸ مقاله برای تحلیل نهایی انتخاب شدند. بیشترین دامنه انتشار مقالات منتخب در ۱۰ سال اخیر بودند و از نظر منابع مواجهه بهترتیب هوا، غذا و آب شرب شایعترین منبع بررسی شده بودند، در حالیکه برای خاک و رسوبات هیچ مطالعهای یافت نشد. بیشترین آلایندههای مورد ارزیابی شامل PAHها، بنزن و BTEX بودند. در حدود نیمی از مطالعات، ارتباط مثبت و معنیدار بین مواجهه با برخی از EDCها و بروز علائم ADHD گزارش شد، در حالیکه سایر مطالعات چنین ارتباطی را نیافتند.
نتیجهگیری: یافتههای این مرور نشان میدهد که اگرچه شواهد رو به رشدی از ارتباط بالقوه بین مواجهه محیطی با EDCها و افزایش خطر ADHD وجود دارد، اما تعداد مطالعات محدود و وجود برخی ناهمگنیها مانع از نتیجهگیری قطعی میشود. این مطالعه ضرورت طراحی پژوهشهای آینده با رویکرد طولی و ارزیابی مواجهه چندمنبعی با کنترل متغیرهای مخدوشکننده را برجسته میسازد. همچنین، توجه به منابع کمتر بررسیشده مانند خاک و رسوبات میتواند به درک جامعتر از مسیرهای واقعی مواجهه و پیامدهای رشد عصبی کودکان کمک کند.
واژههای کلیدی: پایش محیطی، مواجهه، مختلکننده غدد درونریز، اختلال نقص توجه- بیشفعالی، مرور نظاممند
نوع مطالعه: مرور سیستماتیک و فراتحلیل |
موضوع مقاله:
دستگاه اعصاب
دریافت: 1404/5/4 | پذیرش: 1404/9/4 | انتشار: 1404/10/6
دریافت: 1404/5/4 | پذیرش: 1404/9/4 | انتشار: 1404/10/6
فهرست منابع
1. Shah BB. ADHD: Analysis, Statistics, Treatment Approaches and Shortage. J Neurol Res Rev Rep 2022; 4(6): 1-4. [DOI]
2. Wolraich ML, Hagan Jr JF, Allan C, et al. Clinical practice guideline for the diagnosis, evaluation, and treatment of attention-deficit/hyperactivity disorder in children and adolescents. Pediatrics 2019; 144(4): e20192528. [DOI]
3. Silva LA ER, Sousa GD, Migliorini N, et al. Signs and symptoms of Attention Deficit Hyperactivity Disorder and its main comorbidities: A systematic review. Int Seven J Health Res 2023; 2(6): 1386-97. [DOI]
4. Al-Wardat M, Etoom M, Almhdawi KA, et al. Prevalence of attention-deficit hyperactivity disorder in children, adolescents and adults in the Middle East and North Africa region: a systematic review and meta-analysis. BMJ open 2024; 14(1): e078849. [DOI]
5. Popit S, Serod K, Locatelli I, et al. Prevalence of attention-deficit hyperactivity disorder (ADHD): systematic review and meta-analysis. European Psychiatry 2024; 67(1): e68. [DOI]
6. Smith KT. ADHD in Children and Adolescents: Barriers to Ethical and Successful Treatment. J Biosci Med 2023; 11(3): 58-63. [DOI]
7. Wong AW, Landes SD. Expanding understanding of racialethnic differences in ADHD prevalence rates among children to include Asians and Alaskan Natives/American Indians. J Atten Dis 2022; 26(5): 747-54. [DOI]
8. Ayano G, Tsegay L, Gizachew Y, et al. The global prevalence of attention deficit hyperactivity disorder in children and adolescents: An umbrella review of meta-analyses. J Affect Disord 2023; 339: 860-66. [DOI]
9. Xu G, Strathearn L, Liu B, et al. Twenty-year trends in diagnosed attention-deficit/hyperactivity disorder among US children and adolescents, 1997-2016. JAMA network open 2018; 1(4): e181471. [DOI]
10. Faraone S, Biederman J. Pathophysiology of attention-deficit/hyperactivity disorder. Neuropsycho-pharmacology: The fifth generation of progress 2002: 577-96. [Article]
11. Cuffe SP, Visser SN, Holbrook JR, et al. ADHD and psychiatric comorbidity: Functional outcomes in a school-based sample of children. J Atten Dis 2020; 24(9): 1345-54. [DOI]
12. Luo Y, Weibman D, Halperin JM, et al. A review of heterogeneity in attention deficit/hyperactivity disorder (ADHD). Front Hum Neurosci 2019; 13: 42. [DOI]
13. Brunkhorst-Kanaan N, Libutzki B, Reif A, et al. ADHD and accidents over the life span–A systematic review. Neurosci Biobehav Rev 2021; 125: 582-91. [DOI]
14. Luderer M, Quiroga JAR, Faraone SV, et al. Alcohol use disorders and ADHD. Neurosci Biobehav Rev 2021; 128: 648-60. [DOI]
15. Zarei A, Bagherzadeh R, Gharibi T, et al. Tendency to High-Risk Behaviors in Adoles-cents and its Related Factors in Bushehr, 2019. Iran South Med J 2020; 23(6): 554-68. [DOI]
16. Ali AY, Inyang B, Koshy FS, et al. Elements that influence the development of attention deficit hyperactivity disorder (ADHD) in children. Cureus 2022; 14(8): e27835. [DOI]
17. Kanarik M, Grimm O, Mota NR, et al. ADHD co-morbidities: A review of implication of gene× environment effects with dopamine-related genes. Neurosci Biobehav Rev 2022; 139: 104757. [DOI]
18. Demontis D, Walters GB, Athanasiadis G, et al. Genome-wide analyses of ADHD identify 27 risk loci, refine the genetic architecture and implicate several cognitive domains. Nat Genet 2023; 55(2): 198-208. [DOI]
19. Gujska JH, Silczuk A, Madejek R, et al. Exploring the link between attention-deficit hyperactivity disorder and cannabis use disorders: a review. Med Sci Monit 2023; 29: e939749. [DOI]
20. Driga A-M, Drigas A. ADHD in the Early Years: Pre-Natal and Early Causes and Alternative Ways of Dealing. Int J of Online Biomed Eng 2019;15(13): 95-102. [DOI]
21. Kim JH, Kim JY, Lee J, et al. Environmental risk factors, protective factors, and peripheral biomarkers for ADHD: an umbrella review. Lancet Psychiatry 2020; 7(11): 955-70. [DOI]
22. Min X, Li C, Yan Y. Parental age and the risk of ADHD in offspring: a systematic review and meta-analysis. International Int J Environ Res Public Health 2021; 18(9): 4939. [DOI]
23. Shen F, Zhou H. Advances in the etiology and neuroimaging of children with attention deficit hyperactivity disorder. Front Pediatr 2024; 12: 1400468. [DOI]
24. Moore S, Paalanen L, Melymuk L, et al. The associa-tion between ADHD and environmental chemicals—a scoping review. Int J Environ Res Public Health 2022; 19(5): 2849. [DOI]
25. Rivollier F, Krebs M-O, Kebir O. Perinatal exposure to environmental endocrine disruptors in the emergence of neurodevelopmental psychiatric diseases: a systematic review. Int J Environ Res Public Health 2019; 16(8): 1318. [DOI]
26. NIEHS. Endocrine Disruptors: National Institute of Environmental Health Sciences. 2024. [Article]
27. Mughal BB, Fini J-B, Demeneix BA. Thyroid-disrupting chemicals and brain development: an update. Endocrine connections 2018; 7(4): R160-R86. [DOI]
28. Pessah IN, Lein PJ, Seegal RF, et al. Neurotoxicity of polychlorinated biphenyls and related organohalo-gens. Acta Neuropathol 2019; 138(3): 363-87. [DOI]
29. Di Criscio M, Lodahl JE, Stamatakis A, et al. A human-relevant mixture of endocrine disrupting chemicals induces changes in hippocampal DNA methyla-tion correlating with hyperactive behavior in male mice. Chemosphere 2023; 313: 137633. [DOI]
30. Kim JI, Lee YA, Shin CH, et al. Association of bisphenol A, bisphenol F, and bisphenol S with ADHD symptoms in children. Environ Int 2022; 161: 107093. [DOI]
31. Cediel-Ulloa A, Lupu DL, Johansson Y, et al. Impact of endocrine disrupting chemicals on neurodevelopment: the need for better testing strategies for endocrine disruption-induced developmental neurotoxicity. Expert Rev Endocrinol Metab 2022; 17(2): 131-41. [DOI]
32. Schug TT, Blawas AM, Gray K, et al. Elucidating the links between endocrine disruptors and neurodevelopment. Endocrinology 2015; 156(6): 1941-51. [DOI]
33. Shoaff JR, Coull B, Weuve J, et al. Association of exposure to endocrine-disrupting chemicals during adolescence with attention-deficit/hyperactivity disorder–related behaviors. JAMA Netw Open 2020; 3(8): e2015041. [DOI]
34. D'Arrigo T. Endocrine-Disrupting Chemicals Linked to ADHD Behaviors in Adolescents. Psychiatric News 2020; 55(21): 1. [DOI]
35. Yeo K-E, Lim S, Kim A, et al. Association Between Endocrine-Disrupting Chemicals Exposure and Attention-Deficit/Hyperactivity Disorder Symptoms in Children With Attention-Deficit/Hyperactivity Disorder. J Korean Acad Child Adolesc Psychiatry 2025; 36(1): 18. [DOI]
36. Lopez-Garcia M, Martinez-Bebia M, Lopez-Moro A, et al. Endocrine Disruptors and Attention Deficit Hyperactivity Disorder: A Systematic Review. Arch Med Res 2025; 56(7): 103260. [DOI]
37. Wan T, Jun H, Pan W, et al. Kappa coefficient: a popular measure of rater agreement. Shanghai Shanghai Arch Psychiatry 2015; 27(1): 62-7. [DOI]
38. Kou X, Canals J, Bulló M, et al. Association of Prenatal Dietary Toxicants and Inorganic Arsenic Exposure with Children’s Emotional and Behavioral Problems: ECLIPSES Study. Toxics 2024; 12(6): 398. [DOI]
39. Peterson BS, Bansal R, Sawardekar S, et al. Prenatal exposure to air pollution is associated with altered brain structure, function, and metabolism in child-hood. J Child Psychol Psychiatry 2022; 63(11): 1316-31. [DOI]
40. Huang C-c, Pan S-c, Chin W-s, et al. Living proximity to petrochemical industries and the risk of attention-deficit/hyperactivity disorder in children. Environ Res 2022; 212: 113128. [DOI]
41. Dellefratte K, Stingone JA, Claudio L. Combined as-sociation of BTEX and material hardship on ADHD‐suggestive behaviours among a nationally representative sample of US children. Paediatr Perinat Epidemiol 2019; 33(6): 482-9. [DOI]
42. Mortamais M, Pujol J, Van Drooge BL, et al. Effect of exposure to polycyclic aromatic hydrocarbons on basal ganglia and attention-deficit hyperactivity disorder symptoms in primary school children. Environ Int 2017; 105: 12-9. [DOI]
43. Caspersen IH, Aase H, Biele G, et al. The influence of maternal dietary exposure to dioxins and PCBs during pregnancy on ADHD symptoms and cognitive functions in Norwegian preschool children. Environ Int 2016; 94: 649-60. [DOI]
44. Peterson BS, Rauh VA, Bansal R, et al. Effects of prenatal exposure to air pollutants (polycyclic aromatic hydrocarbons) on the development of brain white matter, cognition, and behavior in later childhood. JAMA psychiatry 2015; 72(6): 531-40. [DOI]
45. Chang S, Crothers C, Lai S, et al. Pediatric neurobehavioral diseases in Nevada counties with respect to perchlorate in drinking water: an ecological inquiry. Birth Defects Res A Clin Mol Teratol 2003; 67(10): 886-92. [DOI]
46. Cortese S, Sabé M, Chen C, et al. Half a century of research on attention-deficit/hyperactivity disorder: a scientometric study. Neurosci Biobehav Rev 2022; 140: 104769. [DOI]
47. Dahiya S, Dahiya VT. Mapping The Social Structure Of Attention Deficit Hyperactivity Disorder: A Bibliometric Study. Library Progress International 2024; 44(3): 9774-9786. [DOI]
48. Yaglova N, Yaglov V. Endocrine Disruptors as a New Etiologic Factor of Bone Tissue Diseases (Review). Sovrem Tekhnologii Med 2021; 13(2): 84-94. [DOI]
49. Bimonte V, Besharat Z, Antonioni A, et al. The endocrine disruptor cadmium: a new player in the pathophysiology of metabolic diseases. J Endocrinol In-vest 2021; 44(7): 1363-77. [DOI]
50. Zhang X, Flaws JA, Spinella MJ, et al. The relation-ship between typical environmental endocrine disruptors and kidney disease. Toxics 2022; 11(1): 32. [DOI]
51. Zhang H, Feng S, Song S, et al. First evidence in the association of phenolic endocrine-disrupting chemicals with secondary non-alcoholic fatty liver dis-ease: A case-control study in South China. Environ Pollut 2025; 373: 126086. [DOI]
52. Aghaei M, Yunesian M. Exposure assessment to environmental pollutants in human health risk assessment studies; Overview on new approaches. J Health 2019; 10(2): 138-55. [DOI]
53. Schmidt CW. Monitoring environmental exposures: now it’s personal. Environ Health Perspect; 2006; 114(9): A528–A534. [DOI]
54. del Río Barrera T, Ledesma KNZ, et al. Endocrine Disruptors and Their Impact on Quality of Life: A Literature Review. Cureus 2025; 17(5): e83890. [DOI]
55. Kumar M, Sarma DK, Shubham S, et al. Environmental endocrine-disrupting chemical exposure: role in non-communicable diseases. Front Public Health 2020; 8: 553850. [DOI]
56. Zhang H, Ouyang W, He K, et al. Developing water quality and land use surrogates to predict endocrine-disrupting chemical profiles in a highly urbanized river basin. Environ Pollut 2024; 362: 124951. [DOI]
57. Ravanipour M, Ravanipour M, Hamidi A. The Role of Environmental Health in the Prevention and Control of Environment-Related Diseases Worldwide. Research Square 2024. [DOI]
58. Hamidi A, Ravanipour M, Ravanipour M. The role of environmental health in the prevention and control of diseases related to environmental factors in Iran: a scientometric study. Iran J of Health Environ 2024; 17(2): 221-44. [Article]
59. Hatami G, Eghbali SS, Darki A, Mohebbi G, Mohebbi F, Motamed N. Serum Levels of Lead in 6-7 Year Old Children in Bushehr in 2012. Iran South Med J 2019; 21(6): 459-71. [Article]
60. Jiang J, Zhang L, Wang Z, et al. Spatial consistency of co-exposure to air and surface water pollution and cancer in China. Nat Commun 2024; 15(1): 7813. [DOI]
61. Qi Y, Chen Y, Yan X, et al. Co-exposure of ambient particulate matter and airborne transmission pathogens: the impairment of the upper respiratory sys-tems. Environ Sci Technol. 2022; 56(22): 15892-901. [DOI]
62. Wang J, Wang W, Zhang W, et al. Co-exposure to multiple air pollutants and sleep disordered breathing in patients with or without obstructive sleep apnea: A crosssectional study. Environ Res 2022; 212: 113155. [DOI]
63. Deng Q, Dai X, Feng W, et al. Co-exposure to metals and polycyclic aromatic hydrocarbons, microRNA expression, and early health damage in coke oven workers. Environ Int. 2019; 122: 369-80. [DOI]
ارسال پیام به نویسنده مسئول
| بازنشر اطلاعات | |
 |
این مقاله تحت شرایط Creative Commons Attribution-NonCommercial 4.0 International License قابل بازنشر است. |