Volume 28, Issue 3 (Iran South Med J 2025)
Iran South Med J 2025, 28(3): 724-743 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Mazarei Z, Hamidi A, Ravanipour M, Omrani A, Ravanipour M. Endocrine Disruptors and Attention Deficit Hyperactivity Disorder: A Systematic Review of Environmental Monitoring Exposure Studies. Iran South Med J 2025; 28 (3) :724-743
URL: http://ismj.bpums.ac.ir/article-1-2345-en.html
URL: http://ismj.bpums.ac.ir/article-1-2345-en.html
1- Department of Medicine, School of Medicine, Bushehr University of Medical Sciences, Bushehr, Iran
2- Department of Medical Library & Information Sciences, School of Paramedicine, Bushehr University of Medical Sciences, Bushehr, Iran
3- Department of Nursing, School of Nursing and Midwifery, Bushehr University of Medical Sciences, Bushehr, Iran
The Persian Gulf Tropical Medicine Research Center, The Persian Gulf Biomedical Sciences Research Institute, Bushehr University of Medical Sciences, Bushehr, Iran
4- Department of Pediatrics, School of Medicine, Bushehr University of Medical Sciences, Bushehr, Iran
5- Department of Environmental Health Engineering, School of Health and Nutrition, Bushehr University of Medical Sciences, Bushehr, Iran ,ravan.mas@gmail.com
2- Department of Medical Library & Information Sciences, School of Paramedicine, Bushehr University of Medical Sciences, Bushehr, Iran
3- Department of Nursing, School of Nursing and Midwifery, Bushehr University of Medical Sciences, Bushehr, Iran
The Persian Gulf Tropical Medicine Research Center, The Persian Gulf Biomedical Sciences Research Institute, Bushehr University of Medical Sciences, Bushehr, Iran
4- Department of Pediatrics, School of Medicine, Bushehr University of Medical Sciences, Bushehr, Iran
5- Department of Environmental Health Engineering, School of Health and Nutrition, Bushehr University of Medical Sciences, Bushehr, Iran ,
Abstract: (272 Views)
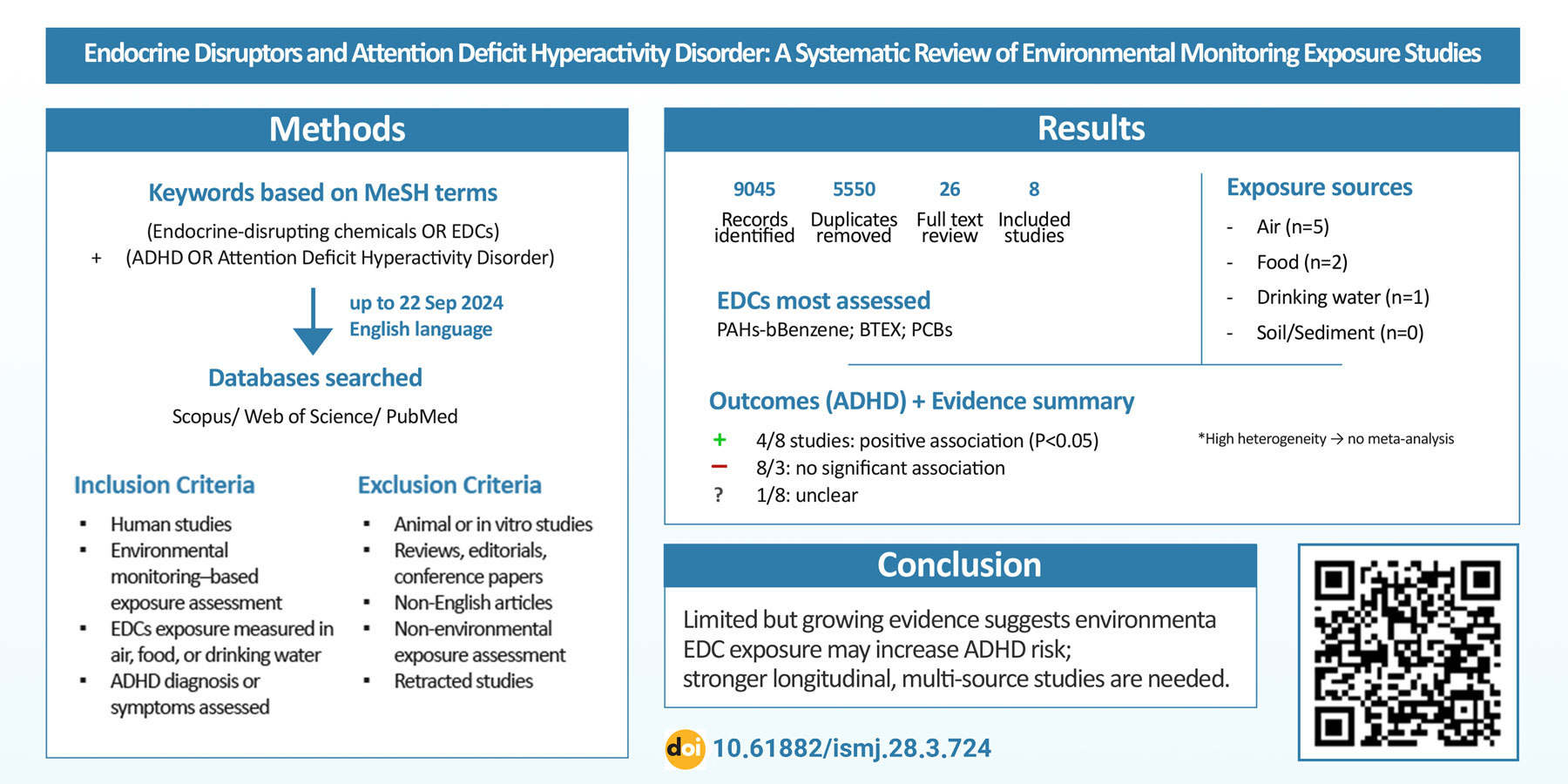
Background: Attention deficit hyperactivity disorder (ADHD) is one of the most common neurodevelopmental disorders in children, with a multifactorial and complex etiology. Recent evidence suggests a combined role of factors, especially endocrine-disrupting chemicals (EDCs), as effective environmental factors in the development of this disorder by disrupting hormonal regulatory pathways and neurodevelopment. Despite the growth of studies in this field, there is still insufficient evidence about the relationship between environmental exposure to EDCs (based on environmental monitoring) and the development of ADHD. Therefore, this systematic review was conducted to determine the existing evidence about the relationship between exposure through environmental monitoring to EDCs and the development of ADHD symptoms.
Materials and Methods: The present study is a systematic review conducted in accordance with the PRISMA checklist. All research articles in English without publication time limit until September 22, 2024 were searched in three databases: Scopus, Web of Science, and PubMed using keywords related to the topic and based on MeSH terms. All stages of screening of articles were performed based on inclusion and exclusion criteria. Finally, the required data were extracted from the final retrieved articles.
Results: Out of 9045 search results, 3495 duplicates were removed and after a complete review of the literature, 8 articles were finally selected for the final analysis. The largest publication range of the selected articles was in the last 10 years and in terms of exposure sources, air, food and drinking water were the most common sources examined, respectively, while no studies were found for soil and sediment. The most frequently evaluated pollutants included PAHs, benzene, and BTEX. About half of the studies reported a positive and significant association between exposure to some EDCs and the occurrence of ADHD symptoms, while other studies did not find such an association.
Conclusion: The findings of this review indicate that although there is growing evidence of a potential association between environmental exposure to EDCs and an increased risk of ADHD, the limited number of studies and the presence of some heterogeneity prevent definitive
conclusions. This study highlights the need for future longitudinal research designs and multi-source exposure assessments that control for confounding variables. Also, focusing on less studied sources such as soil and sediments may contribute to a more comprehensive understanding of the actual exposure pathways and neurodevelopmental outcomes in children.
Materials and Methods: The present study is a systematic review conducted in accordance with the PRISMA checklist. All research articles in English without publication time limit until September 22, 2024 were searched in three databases: Scopus, Web of Science, and PubMed using keywords related to the topic and based on MeSH terms. All stages of screening of articles were performed based on inclusion and exclusion criteria. Finally, the required data were extracted from the final retrieved articles.
Results: Out of 9045 search results, 3495 duplicates were removed and after a complete review of the literature, 8 articles were finally selected for the final analysis. The largest publication range of the selected articles was in the last 10 years and in terms of exposure sources, air, food and drinking water were the most common sources examined, respectively, while no studies were found for soil and sediment. The most frequently evaluated pollutants included PAHs, benzene, and BTEX. About half of the studies reported a positive and significant association between exposure to some EDCs and the occurrence of ADHD symptoms, while other studies did not find such an association.
Conclusion: The findings of this review indicate that although there is growing evidence of a potential association between environmental exposure to EDCs and an increased risk of ADHD, the limited number of studies and the presence of some heterogeneity prevent definitive
conclusions. This study highlights the need for future longitudinal research designs and multi-source exposure assessments that control for confounding variables. Also, focusing on less studied sources such as soil and sediments may contribute to a more comprehensive understanding of the actual exposure pathways and neurodevelopmental outcomes in children.
Keywords: Attention Deficit Hyperactivity Disorder, Endocrine Disruptor, Environmental Monitoring, Exposure, Systematic Review
Type of Study: Review Systematic and Meta Analysis |
Subject:
Nervous System
Received: 2025/07/26 | Accepted: 2025/11/25 | Published: 2025/12/27
Received: 2025/07/26 | Accepted: 2025/11/25 | Published: 2025/12/27
References
1. Shah BB. ADHD: Analysis, Statistics, Treatment Approaches and Shortage. J Neurol Res Rev Rep 2022; 4(6): 1-4. [DOI]
2. Wolraich ML, Hagan Jr JF, Allan C, et al. Clinical practice guideline for the diagnosis, evaluation, and treatment of attention-deficit/hyperactivity disorder in children and adolescents. Pediatrics 2019; 144(4): e20192528. [DOI]
3. Silva LA ER, Sousa GD, Migliorini N, et al. Signs and symptoms of Attention Deficit Hyperactivity Disorder and its main comorbidities: A systematic review. Int Seven J Health Res 2023; 2(6): 1386-97. [DOI]
4. Al-Wardat M, Etoom M, Almhdawi KA, et al. Prevalence of attention-deficit hyperactivity disorder in children, adolescents and adults in the Middle East and North Africa region: a systematic review and meta-analysis. BMJ open 2024; 14(1): e078849. [DOI]
5. Popit S, Serod K, Locatelli I, et al. Prevalence of attention-deficit hyperactivity disorder (ADHD): systematic review and meta-analysis. European Psychiatry 2024; 67(1): e68. [DOI]
6. Smith KT. ADHD in Children and Adolescents: Barriers to Ethical and Successful Treatment. J Biosci Med 2023; 11(3): 58-63. [DOI]
7. Wong AW, Landes SD. Expanding understanding of racialethnic differences in ADHD prevalence rates among children to include Asians and Alaskan Natives/American Indians. J Atten Dis 2022; 26(5): 747-54. [DOI]
8. Ayano G, Tsegay L, Gizachew Y, et al. The global prevalence of attention deficit hyperactivity disorder in children and adolescents: An umbrella review of meta-analyses. J Affect Disord 2023; 339: 860-66. [DOI]
9. Xu G, Strathearn L, Liu B, et al. Twenty-year trends in diagnosed attention-deficit/hyperactivity disorder among US children and adolescents, 1997-2016. JAMA network open 2018; 1(4): e181471. [DOI]
10. Faraone S, Biederman J. Pathophysiology of attention-deficit/hyperactivity disorder. Neuropsycho-pharmacology: The fifth generation of progress 2002: 577-96. [Article]
11. Cuffe SP, Visser SN, Holbrook JR, et al. ADHD and psychiatric comorbidity: Functional outcomes in a school-based sample of children. J Atten Dis 2020; 24(9): 1345-54. [DOI]
12. Luo Y, Weibman D, Halperin JM, et al. A review of heterogeneity in attention deficit/hyperactivity disorder (ADHD). Front Hum Neurosci 2019; 13: 42. [DOI]
13. Brunkhorst-Kanaan N, Libutzki B, Reif A, et al. ADHD and accidents over the life span–A systematic review. Neurosci Biobehav Rev 2021; 125: 582-91. [DOI]
14. Luderer M, Quiroga JAR, Faraone SV, et al. Alcohol use disorders and ADHD. Neurosci Biobehav Rev 2021; 128: 648-60. [DOI]
15. Zarei A, Bagherzadeh R, Gharibi T, et al. Tendency to High-Risk Behaviors in Adoles-cents and its Related Factors in Bushehr, 2019. Iran South Med J 2020; 23(6): 554-68. [DOI]
16. Ali AY, Inyang B, Koshy FS, et al. Elements that influence the development of attention deficit hyperactivity disorder (ADHD) in children. Cureus 2022; 14(8): e27835. [DOI]
17. Kanarik M, Grimm O, Mota NR, et al. ADHD co-morbidities: A review of implication of gene× environment effects with dopamine-related genes. Neurosci Biobehav Rev 2022; 139: 104757. [DOI]
18. Demontis D, Walters GB, Athanasiadis G, et al. Genome-wide analyses of ADHD identify 27 risk loci, refine the genetic architecture and implicate several cognitive domains. Nat Genet 2023; 55(2): 198-208. [DOI]
19. Gujska JH, Silczuk A, Madejek R, et al. Exploring the link between attention-deficit hyperactivity disorder and cannabis use disorders: a review. Med Sci Monit 2023; 29: e939749. [DOI]
20. Driga A-M, Drigas A. ADHD in the Early Years: Pre-Natal and Early Causes and Alternative Ways of Dealing. Int J of Online Biomed Eng 2019;15(13): 95-102. [DOI]
21. Kim JH, Kim JY, Lee J, et al. Environmental risk factors, protective factors, and peripheral biomarkers for ADHD: an umbrella review. Lancet Psychiatry 2020; 7(11): 955-70. [DOI]
22. Min X, Li C, Yan Y. Parental age and the risk of ADHD in offspring: a systematic review and meta-analysis. International Int J Environ Res Public Health 2021; 18(9): 4939. [DOI]
23. Shen F, Zhou H. Advances in the etiology and neuroimaging of children with attention deficit hyperactivity disorder. Front Pediatr 2024; 12: 1400468. [DOI]
24. Moore S, Paalanen L, Melymuk L, et al. The associa-tion between ADHD and environmental chemicals—a scoping review. Int J Environ Res Public Health 2022; 19(5): 2849. [DOI]
25. Rivollier F, Krebs M-O, Kebir O. Perinatal exposure to environmental endocrine disruptors in the emergence of neurodevelopmental psychiatric diseases: a systematic review. Int J Environ Res Public Health 2019; 16(8): 1318. [DOI]
26. NIEHS. Endocrine Disruptors: National Institute of Environmental Health Sciences. 2024. [Article]
27. Mughal BB, Fini J-B, Demeneix BA. Thyroid-disrupting chemicals and brain development: an update. Endocrine connections 2018; 7(4): R160-R86. [DOI]
28. Pessah IN, Lein PJ, Seegal RF, et al. Neurotoxicity of polychlorinated biphenyls and related organohalo-gens. Acta Neuropathol 2019; 138(3): 363-87. [DOI]
29. Di Criscio M, Lodahl JE, Stamatakis A, et al. A human-relevant mixture of endocrine disrupting chemicals induces changes in hippocampal DNA methyla-tion correlating with hyperactive behavior in male mice. Chemosphere 2023; 313: 137633. [DOI]
30. Kim JI, Lee YA, Shin CH, et al. Association of bisphenol A, bisphenol F, and bisphenol S with ADHD symptoms in children. Environ Int 2022; 161: 107093. [DOI]
31. Cediel-Ulloa A, Lupu DL, Johansson Y, et al. Impact of endocrine disrupting chemicals on neurodevelopment: the need for better testing strategies for endocrine disruption-induced developmental neurotoxicity. Expert Rev Endocrinol Metab 2022; 17(2): 131-41. [DOI]
32. Schug TT, Blawas AM, Gray K, et al. Elucidating the links between endocrine disruptors and neurodevelopment. Endocrinology 2015; 156(6): 1941-51. [DOI]
33. Shoaff JR, Coull B, Weuve J, et al. Association of exposure to endocrine-disrupting chemicals during adolescence with attention-deficit/hyperactivity disorder–related behaviors. JAMA Netw Open 2020; 3(8): e2015041. [DOI]
34. D'Arrigo T. Endocrine-Disrupting Chemicals Linked to ADHD Behaviors in Adolescents. Psychiatric News 2020; 55(21): 1. [DOI]
35. Yeo K-E, Lim S, Kim A, et al. Association Between Endocrine-Disrupting Chemicals Exposure and Attention-Deficit/Hyperactivity Disorder Symptoms in Children With Attention-Deficit/Hyperactivity Disorder. J Korean Acad Child Adolesc Psychiatry 2025; 36(1): 18. [DOI]
36. Lopez-Garcia M, Martinez-Bebia M, Lopez-Moro A, et al. Endocrine Disruptors and Attention Deficit Hyperactivity Disorder: A Systematic Review. Arch Med Res 2025; 56(7): 103260. [DOI]
37. Wan T, Jun H, Pan W, et al. Kappa coefficient: a popular measure of rater agreement. Shanghai Shanghai Arch Psychiatry 2015; 27(1): 62-7. [DOI]
38. Kou X, Canals J, Bulló M, et al. Association of Prenatal Dietary Toxicants and Inorganic Arsenic Exposure with Children’s Emotional and Behavioral Problems: ECLIPSES Study. Toxics 2024; 12(6): 398. [DOI]
39. Peterson BS, Bansal R, Sawardekar S, et al. Prenatal exposure to air pollution is associated with altered brain structure, function, and metabolism in child-hood. J Child Psychol Psychiatry 2022; 63(11): 1316-31. [DOI]
40. Huang C-c, Pan S-c, Chin W-s, et al. Living proximity to petrochemical industries and the risk of attention-deficit/hyperactivity disorder in children. Environ Res 2022; 212: 113128. [DOI]
41. Dellefratte K, Stingone JA, Claudio L. Combined as-sociation of BTEX and material hardship on ADHD‐suggestive behaviours among a nationally representative sample of US children. Paediatr Perinat Epidemiol 2019; 33(6): 482-9. [DOI]
42. Mortamais M, Pujol J, Van Drooge BL, et al. Effect of exposure to polycyclic aromatic hydrocarbons on basal ganglia and attention-deficit hyperactivity disorder symptoms in primary school children. Environ Int 2017; 105: 12-9. [DOI]
43. Caspersen IH, Aase H, Biele G, et al. The influence of maternal dietary exposure to dioxins and PCBs during pregnancy on ADHD symptoms and cognitive functions in Norwegian preschool children. Environ Int 2016; 94: 649-60. [DOI]
44. Peterson BS, Rauh VA, Bansal R, et al. Effects of prenatal exposure to air pollutants (polycyclic aromatic hydrocarbons) on the development of brain white matter, cognition, and behavior in later childhood. JAMA psychiatry 2015; 72(6): 531-40. [DOI]
45. Chang S, Crothers C, Lai S, et al. Pediatric neurobehavioral diseases in Nevada counties with respect to perchlorate in drinking water: an ecological inquiry. Birth Defects Res A Clin Mol Teratol 2003; 67(10): 886-92. [DOI]
46. Cortese S, Sabé M, Chen C, et al. Half a century of research on attention-deficit/hyperactivity disorder: a scientometric study. Neurosci Biobehav Rev 2022; 140: 104769. [DOI]
47. Dahiya S, Dahiya VT. Mapping The Social Structure Of Attention Deficit Hyperactivity Disorder: A Bibliometric Study. Library Progress International 2024; 44(3): 9774-9786. [DOI]
48. Yaglova N, Yaglov V. Endocrine Disruptors as a New Etiologic Factor of Bone Tissue Diseases (Review). Sovrem Tekhnologii Med 2021; 13(2): 84-94. [DOI]
49. Bimonte V, Besharat Z, Antonioni A, et al. The endocrine disruptor cadmium: a new player in the pathophysiology of metabolic diseases. J Endocrinol In-vest 2021; 44(7): 1363-77. [DOI]
50. Zhang X, Flaws JA, Spinella MJ, et al. The relation-ship between typical environmental endocrine disruptors and kidney disease. Toxics 2022; 11(1): 32. [DOI]
51. Zhang H, Feng S, Song S, et al. First evidence in the association of phenolic endocrine-disrupting chemicals with secondary non-alcoholic fatty liver dis-ease: A case-control study in South China. Environ Pollut 2025; 373: 126086. [DOI]
52. Aghaei M, Yunesian M. Exposure assessment to environmental pollutants in human health risk assessment studies; Overview on new approaches. J Health 2019; 10(2): 138-55. [DOI]
53. Schmidt CW. Monitoring environmental exposures: now it’s personal. Environ Health Perspect; 2006; 114(9): A528–A534. [DOI]
54. del Río Barrera T, Ledesma KNZ, et al. Endocrine Disruptors and Their Impact on Quality of Life: A Literature Review. Cureus 2025; 17(5): e83890. [DOI]
55. Kumar M, Sarma DK, Shubham S, et al. Environmental endocrine-disrupting chemical exposure: role in non-communicable diseases. Front Public Health 2020; 8: 553850. [DOI]
56. Zhang H, Ouyang W, He K, et al. Developing water quality and land use surrogates to predict endocrine-disrupting chemical profiles in a highly urbanized river basin. Environ Pollut 2024; 362: 124951. [DOI]
57. Ravanipour M, Ravanipour M, Hamidi A. The Role of Environmental Health in the Prevention and Control of Environment-Related Diseases Worldwide. Research Square 2024. [DOI]
58. Hamidi A, Ravanipour M, Ravanipour M. The role of environmental health in the prevention and control of diseases related to environmental factors in Iran: a scientometric study. Iran J of Health Environ 2024; 17(2): 221-44. [Article]
59. Hatami G, Eghbali SS, Darki A, Mohebbi G, Mohebbi F, Motamed N. Serum Levels of Lead in 6-7 Year Old Children in Bushehr in 2012. Iran South Med J 2019; 21(6): 459-71. [Article]
60. Jiang J, Zhang L, Wang Z, et al. Spatial consistency of co-exposure to air and surface water pollution and cancer in China. Nat Commun 2024; 15(1): 7813. [DOI]
61. Qi Y, Chen Y, Yan X, et al. Co-exposure of ambient particulate matter and airborne transmission pathogens: the impairment of the upper respiratory sys-tems. Environ Sci Technol. 2022; 56(22): 15892-901. [DOI]
62. Wang J, Wang W, Zhang W, et al. Co-exposure to multiple air pollutants and sleep disordered breathing in patients with or without obstructive sleep apnea: A crosssectional study. Environ Res 2022; 212: 113155. [DOI]
63. Deng Q, Dai X, Feng W, et al. Co-exposure to metals and polycyclic aromatic hydrocarbons, microRNA expression, and early health damage in coke oven workers. Environ Int. 2019; 122: 369-80. [DOI]
Send email to the article author
| Rights and Permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |