Volume 28, Issue 3 (Iran South Med J 2025)
Iran South Med J 2025, 28(3): 644-653 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Salavatifar M, Joorabli A, Hayati Roodbari N. Simulated Weightlessness Effect on Ovarian Follicular Structure and Estradiol Levels in Rats. Iran South Med J 2025; 28 (3) :644-653
URL: http://ismj.bpums.ac.ir/article-1-2339-en.html
URL: http://ismj.bpums.ac.ir/article-1-2339-en.html
1- Aerospace Physiology Department, Aerospace Research Institute, Ministry of Science, Research and Technology, Tehran, Iran , salavati@ari.ac.ir
2- Biology Department, School of Converging Sciences and Technologies, Science and Research Branch, Islamic Azad Uni-versity, Tehran, Iran
2- Biology Department, School of Converging Sciences and Technologies, Science and Research Branch, Islamic Azad Uni-versity, Tehran, Iran
Abstract: (229 Views)
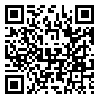
Background: Long-term human habitation in space, enabled by advances in space travel, may impair the function of various physiological systems. Given the critical need to maintain astronauts’ health during and after missions, this study investigated the effects of simulated weightlessness using a hindlimb unloading model in female rats, focusing on reproductive system function.
Materials and Methods: Twenty Wistar rats were divided into two groups: a control group under normal gravity and a simulated weightlessness group subjected to hindlimb unloading for four weeks. Post-intervention, blood estradiol levels, ovarian size, and follicular status (primordial, secondary, Graafian, antral, and corpus luteum follicles) were assessed.
Results: The weightlessness group exhibited a significant increase in estradiol levels, accompanied by a reduction in ovarian size and a decrease in the number of secondary and Graafian follicles. However, the numbers of primordial and antral follicles, as well as the corpus luteum, did not show significant changes.
Conclusion: The results indicated that simulated weightlessness negatively impacts ovarian function and follicular structure. This may affect the fertility of female astronauts. These findings underscore the importance of rigorous monitoring of reproductive health during space missions and the development of preventive strategies to mitigate the physiological disruptions associated with weightlessness.
Materials and Methods: Twenty Wistar rats were divided into two groups: a control group under normal gravity and a simulated weightlessness group subjected to hindlimb unloading for four weeks. Post-intervention, blood estradiol levels, ovarian size, and follicular status (primordial, secondary, Graafian, antral, and corpus luteum follicles) were assessed.
Results: The weightlessness group exhibited a significant increase in estradiol levels, accompanied by a reduction in ovarian size and a decrease in the number of secondary and Graafian follicles. However, the numbers of primordial and antral follicles, as well as the corpus luteum, did not show significant changes.
Conclusion: The results indicated that simulated weightlessness negatively impacts ovarian function and follicular structure. This may affect the fertility of female astronauts. These findings underscore the importance of rigorous monitoring of reproductive health during space missions and the development of preventive strategies to mitigate the physiological disruptions associated with weightlessness.
Type of Study: Original |
Subject:
Physiology
Received: 2025/04/20 | Accepted: 2025/08/10 | Published: 2025/12/27
Received: 2025/04/20 | Accepted: 2025/08/10 | Published: 2025/12/27
References
1. Gimunová M, Paludo AC, Bernaciková M, et al. The effect of space travel on human reproductive health: a systematic review. npj Microgravity 2024; 10(1): 10. [DOI]
2. Mishra B, Luderer U. Reproductive hazards of space travel in women and men. Nat Rev Endocrinol 2019; 15(12): 713-730. [DOI]
3. Strock N, Rivas E, Goebel KM. The effects of space flight and microgravity exposure on female astronaut health and performance. IEEE Aero-space Conference 2023; 1-12. [DOI]
4. Tou J, Ronca A, Grindeland R, et al. Models to study gravitational biology of mammalian repro-duction. Biology of reproduction 2002; 67(6): 1681-1687. [DOI]
5. Vinogradova O, Tomilovskaya E, Kozlovskaya I. Gravity as a factor in evolutionary adaptation of animals to living on the earth. Human Physiology 2021; 47(7): 716-734. [DOI]
6. Mathyk B, Imudia AN, Quaas AM, et al. Understand-ing how space travel affects the female reproduc-tive system to the Moon and beyond. npj Women's Health. 2024; 2(1): 20. [DOI]
7. Lauria L, Ballard TJ, Caldora M, et al. Reproductive disorders and pregnancy outcomes among female flight attendants. Aviat Space Environ Med 2006; 77(5): 533-539. [Article]
8. Radowicka M, Pietrzak B, Wielgoś M. Assessment of the occurrence of menstrual disorders in female flight attendants–preliminary report and literature review. Neuro Endocrinol Lett 2013; 34(8): 809-813. [Article]
9. Rosa‐Caldwell ME, Mortreux M, Kaiser UB, et al. The oestrous cycle and skeletal muscle atrophy: Investigations in rodent models of muscle loss. Experimental physiology 2021; 106(12): 2472-2488. [DOI]
10. Sandler H, Winter DL. Physiological responses of women to simulated weightlessness: a review of the first female bed-rest stud. National Aeronautics and Space Administration 1978. [Article]
11. Cialdai F, Brown AM, Baumann CW, et al. How do gravity alterations affect animal and human systems at a cellular/tissue level? npj Microgravity 2023; 9(1): 84. [DOI]
12. Thornton W, Bonato F. The Human Body and Weightlessness. Springer, 2017; 31-55. [DOI]
13. Cheng K, Feng Xa, Yang C, et al. Simulated micro-gravity reduces quality of ovarian follicles and oocytes by disrupting communications of follicle cells. npj Microgravity 2023; 9(1): 7. [DOI]
14. Wang C, Wu J, Cui Y, et al. Simulated weightless-ness by tail-suspension affects follicle develop-ment and reproductive capacity in rats. Int J Clin Exp Pathol 2016; 9(12): 12208-12218. [Article]
15. Morey-Holton ER, Globus RK. Hindlimb unloading rodent model: technical aspects. Journal of applied physiology 2002; 92(4): 1367-1377. [DOI]
16. Junqueira LC, Mescher AL. Junqueira's basic histology: text & atlas/Anthony L. Mescher: New York [etc.]: McGraw-Hill Medical; 2013. [Article]
17. Cardiff RD, Miller CH, Munn RJ. Manual hematoxy-lin and eosin staining of mouse tissue sections. Cold Spring Harb Protoc 2014; 2014(6): 655-658 [DOI]
18. Picut CA, Dixon D, Simons ML, et al. Postnatal ovary development in the rat: morphologic study and correlation of morphology to neuroendocrine parameters. Toxicologic pathology 2015; 43(3): 343-353. [DOI]
19. He B, Yin X, Hao D, et al. Blockade of IL-6 allevi-ates bone loss induced by modeled microgravity in mice. Can J Physiol Pharmacol 2020; 98(10): 678-83. [DOI]
20. Demontis GC, Germani MM, Caiani EG, et al. Human pathophysiological adaptations to the space environment. Front physiol 2017; 8: 547. [DOI]
21. Mathyk BA, Tabetah M, Karim R, et al. Spaceflight induces changes in gene expression profiles linked to insulin and estrogen. Commun Biol 2024; 7(1): 692. [DOI]
22. Ikeda K, Horie Inoue K, Inoue S. Functions of estrogen and estrogen receptor signaling on skeletal muscle. J Steroid Biochem Mol Biol 2019; 191: 105375. [DOI]
23. Brooke A, Monson J. DHEA and quality of life. Clinical endocrinology 2013; 79(1): 142. [DOI]
24. Shokrani T, Shojaeian NA, Mortazavi A. Effects of High-Intensity Interval Training and Yoga on Serum Estradiol Levels and Sexual Function among Postpartum Women: A Randomized Controlled Trial. Iran South Med J 2024; 26(6): 341-355. [DOI]
25. Kikina AY, Matrosova MS, Gorbacheva EY, et al. Weightlessness leads to an increase granulosa cells in the growing follicle. npj Microgravity 2024; 10(1): 70. [DOI]
26. Hong X, Ratri A, Choi SY, et al. Effects of space-flight aboard the International Space Station on mouse estrous cycle and ovarian gene expression. npj Microgravity 2021; 7(1): 11. [DOI]
27. Zhang S, Zheng D, Wu Y, et al. Simulated micro-gravity using a rotary culture system compromises the in vitro development of mouse preantral follicles. PLoS One 2016: 3(11): e0151062. [DOI]
28. Holets LM, Gupta V, Roby KF, et al. Spaceflight Inhibits Ovarian Follicle Development, Induces Down Regulation of Estrogen Receptor Alpha, and Alters Metabolic Pathways and Gene Expression in Mouse Uterus. Biology of Reproduction 2012; 87(1); 18. [DOI]
Send email to the article author
| Rights and Permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |